We Can’t Treat Homelessness Only in the Emergency Room
Hospitals, ERs, and Police Are Overwhelmed by Homelessness
Homeless encampments like this one are a familiar sight in many cities, reflecting a humanitarian crisis that also puts heavy strain on public systems. As someone who operates a homeless recuperative care program, I see the fallout of treating homelessness as a series of emergencies. Unsheltered individuals often cycle through emergency rooms and hospitals, racking up repeated visits and extended inpatient stays because they have nowhere safe to recover. One study found people experiencing homelessness visited the ER about 6 times per year on average, versus 1.6 times for those with stable housing. nhchc.org. They also tend to stay ~4 days longer per hospital admission, costing over $4,000 more per visit than other patients. nhchc.org. These frequent health crises aren’t because homeless patients want to be in the hospital, it’s because discharge to the street often leads to complications that send them right back.
It’s not just hospitals feeling the burden. Law enforcement and local infrastructure are effectively running triage for homelessness. Police and paramedics respond to untreated medical and mental health crises on the street. Jails become costly default “housing” for minor offenses related to homelessness. In my county, an analysis estimated that around 750 homeless individuals accounted for over $5 million in ambulance rides, ER visits, and jail costs in a single year. Likewise, cities spend millions on encampment clean-ups and emergency shelter measures — for example, California’s transportation agency spent $10 million in one year just to clear about 7,000 highway camps. dot.ca.gov. Taxpayers end up funding this expensive, reactive carousel of 911 calls, hospitalizations, jail stays, and street clean-ups. It’s clear that the status quo of bouncing people between the sidewalk and the emergency room is both inefficient and unsustainable. We need a better approach that stops the revolving door.
A Common-Sense Alternative: Medical Recuperative Care
After years of confronting these crises, We’ve learned there is a better way to break the cycle. Medical recuperative care (also known as medical respite care) provides a structured, short-term place for a homeless patient to recuperate after acute illness or injury. Instead of discharging a sick individual back to a tent under a freeway or keeping them in a costly hospital bed for weeks, hospitals can refer them to a specialized facility where they can rest, recover, and stabilize under medical supervision. The National Institute for Medical Respite Care defines this model as “acute and post-acute care for people experiencing homelessness who are too ill or frail to recover from an illness or injury on the streets or in shelter, but who do not require hospital-level care”. commonwealthfund.org. In practice, that means providing short-term housing with healthcare support typically a stay of a few weeks up to a few months, until the person is well enough to move on. Crucially, recuperative care offers what a shelter or sidewalk cannot: a clean bed, regular meals, help with medications, and a safe environment conducive to healing. It’s an intermediate step that closes the gap between hospital and home. From my vantage point, it’s basically “step-down housing” for someone who is medically vulnerable: far cheaper and more appropriate than a hospital, yet far more supportive than a shelter cot. And it’s proven to work.
Lower Costs, Better Outcomes
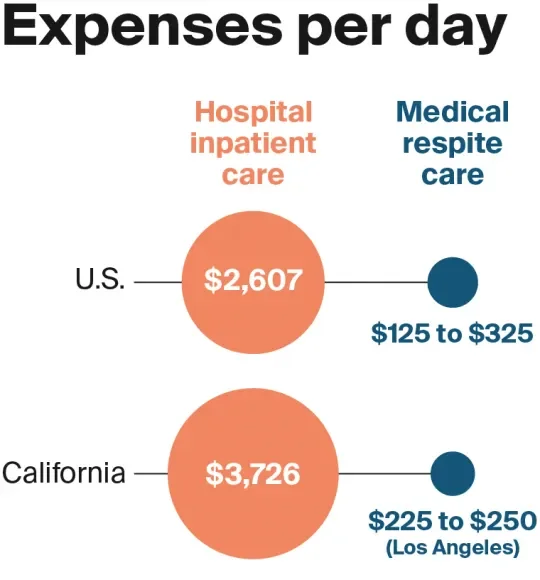
Inpatient hospital care can cost thousands of dollars per day, whereas a recuperative care bed costs only a few hundred. commonwealthfund.org. This stark cost difference has huge implications. In my program, I often remind stakeholders that we can provide about 10 days of recuperative care for the cost of a single day in the hospital. Multiply that across dozens of patients and it’s evident how much money could be saved by treating recuperative care as a standard discharge option. One successful program in Los Angeles estimates it has saved the health care system over $20 million by preventing unnecessarily prolonged hospital stays. commonwealthfund.org. Simply put, it’s a far more cost-effective use of healthcare dollars.
Cost isn’t the only consideration, outcomes are just as important. Recuperative care isn’t about shuttling people out of sight; it’s about improving health and stability, which ultimately reduces the downstream burden on emergency services. A growing body of data (and my own on-the-ground experience) shows that giving patients a place to properly recuperate leads to fewer ER returns and hospital readmissions:
Fewer repeat hospitalizations: In Boston, homeless patients discharged to a medical respite program had 50% lower odds of being readmitted within 90 days compared to those discharged to no support. nhchc.org. I’ve seen this firsthand, when people have a safe place to finish their antibiotics, get wound care, and rest, they are much less likely to bounce back to the hospital.
Reduced hospital days: A Chicago study found that patients who used recuperative care needed dramatically fewer hospital days in the following year (3.4 days vs. 8.1 days) than those who recovered on their own. nhchc.org. In other words, proper post-hospital care cut their hospital usage by more than half.
Lower emergency service use: Overall reviews of medical respite programs show consistent drops in ER visits and inpatient admissions after a respite stay. commonwealthfund.org. As patients stabilize and connect to outpatient care, they rely less on 911 and emergency departments.
Better long-term stability: Importantly, many recuperative care programs help clients secure housing or ongoing support, which leads to improved housing outcomes. commonwealthfund.org. Breaking the homelessness–hospitalization cycle means people are less likely to end up back on the streets (and back in crisis).
The evidence tells a clear story: recuperative care improves health outcomes while containing costs. By providing a controlled environment for recovery, we prevent the kinds of complications and crises that would have required another ambulance ride or another costly ICU admission. From a systems perspective, it’s hard to imagine a more outcome-driven intervention, it keeps people healthier and uses resources more efficiently.
More Than a Bed: Support, Navigation, and Accountability
It’s important to understand that a recuperative care facility is not just a flop house or a makeshift clinic, it’s a deliberately structured environment that pairs housing with health services. In running one of these programs, I’ve seen how crucial the supportive framework is to its success. Guests aren’t simply left to their own devices; we create an organized, accountable setting that helps them rebuild stability step by step.
A well-run recuperative care program typically includes:
24/7 supervision and care: Staff are on-site at all hours to assist clients and respond to any medical issues or emergencies. This continuous oversight ensures safety and helps build trust.
Medical oversight and medication management: Nurses or trained staff monitor each person’s health status, check vital signs, and ensure medications are taken as prescribed. For example, if someone needs daily wound care or insulin, it gets done. This prevents small issues from escalating.
Case management and housing navigation: Dedicated case managers or housing navigators work with each client on an exit plan. That means helping with paperwork (IDs, Medicaid, veteran benefits, etc.), connecting to primary care or mental health providers, and crucially, applying for longer-term housing programs. In some existing models, staff coordinate with housing transition services and even help clients get into subsidized apartments or group housing when they’re ready.
Transportation and appointment coordination: The program helps schedule follow-up medical appointments and often provides rides. This logistical support is key, it keeps people on track with outpatient care that prevents relapse.
Life skills and stability building: Many recuperative care sites offer basic life skills training and require a level of participant responsibility. Clients might attend workshops on budgeting, cooking, or managing their health conditions. They’re typically expected to participate in daily routines (like cleaning their space or checking in with staff). This kind of participant accountability is not about punishment; it’s about preparing people for the expectations of permanent housing and independence.
Structure and rules: Unlike an overnight shelter, recuperative care has a structured routine and some reasonable rules to maintain a safe, healing environment. For instance, programs usually prohibit alcohol or illicit drug use on site and enforce quiet hours. In my experience, guests appreciate having a stable structure after the chaos of the streets it’s a relief to know what to expect each day. Those who refuse to follow basic rules may be discharged, but that’s rare when engagement is high. The structure actually empowers people: it creates a sense of normalcy and personal responsibility that many haven’t experienced in a long time.
In short, recuperative care provides wraparound support. We address immediate medical needs and the underlying issues that led to homelessness. As a program, We approach it like operating a small supportive community: we have nurses, social workers, housing specialists, and often partnerships with local clinics or behavioral health providers. This interdisciplinary approach means we can simultaneously work on a patient’s health, housing, and social stability. When all these pieces come together, the result is someone who leaves our program far better off than when they came in healthier, connected to ongoing care, and often with a housing plan in motion. And importantly, they leave with the confidence that comes from accomplishing goals in a structured setting.
From Emergency Response to Outcome-Focused Care: A Call to Action
We have spent years in the trenches of the homelessness crisis, and one thing is clear: we have to stop treating homelessness primarily as an emergency to react to. The current pattern of camp sweeps, 911 calls, ER visits, repeat arrests is a costly revolving door that fails both the individuals in crisis and the public budget. It’s time for cities and counties to pivot from that reactive mindset to a proactive, systems-focused strategy. Medical recuperative care should be embraced as a standard, not a special experiment, in our continuum of care for homelessness.
This is not about finding a miracle cure or “solving homelessness overnight.” It’s about investing in practical solutions that are proven to work. We know that when people have a safe place to heal and get linked to services, they stabilize. We know it saves money withevery avoided hospitalization or jail booking is money that can be better spent on housing and prevention. And we know it’s scalable: many communities have small medical respite programs, but they remain underfunded and underutilized relative to the need. That needs to change.
As someone who operates a recuperative care program, I call on policymakers and public leaders to make recuperative care a staple in our homelessness response. Fund more beds and programs that integrate medical care with short-term housing and case management. Encourage hospitals to form partnerships with these programs instead of bearing the cost of avoidable long inpatient stays. Include recuperative care as a key element in discharge planning for every homeless patient. And ensure that these programs are connected to the broader housing system so that clients have somewhere to go afterward, whether that’s supportive housing, a sober living home, or a reunification with family.
The homeless crisis is often described as overwhelming, but solutions like recuperative care show that it’s manageable when we operate smarter. We have an opportunity to turn a vicious cycle into a virtuous one: transitioning people from the street, to recovery, to housing. It’s good for the individual and it’s good for the system. The data supports it, and I’ve seen the human success stories behind the data. Let’s stop pouring money into Band-Aid reactions and start investing in integrated, outcome-driven models that treat homelessness as the complex but solvable problem it is. Cities and counties must step up and make medical recuperative care a standard part of the solution because managing homelessness as a perpetual emergency is a path we simply can’t afford, financially or morally, any longer.
Sources: The facts and outcomes cited in this article are drawn from studies and reports on medical respite care and homelessness, including research by the National Health Care for the Homeless Council nhchc.orgnhchc.org, the Commonwealth Fund commonwealthfund.orgcommonwealthfund.org, and other analyses of homelessness costs www2.ljworld.comdot.ca.gov. These demonstrate the cost savings and improved health results when recuperative care is implemented as part of the continuum of care.